News & Blog
Content
- Research Participants Needed
- April 2021 Emphasise capability, not disability: exploring public perceptions, facilitators and barriers to living well with dementia in Northern Ireland
- Feb 2021: New Research Paper Priorities for psychosocial supports and services among family carers of people with dementia in Ireland
- Kathleen Quinlan - Why I take part in research
- January 2021: Dementia Research Network Ireland: Prevention: Cure & Care for Dementia & Neurodegeneration
- December 2020: FDA Reviewing New Alzheimer's Drug
Research Participants Needed
April 2021
Emphasise capability, not disability: exploring public perceptions, facilitators and barriers to living well with dementia in Northern Ireland
Research Intern Angela Miller from The ASI brings us a summary of a research paper led by Dr Gary Mitchell
Background
Understanding of living with dementia has improved but there is a need to expand this knowledge more in the general public to facilitate better quality of life. This call has come from people in all areas of the dementia care community. The capabilities approach aims to promote wellbeing by encouraging people to realise their capabilities and engage in things they value.
What the research team did
Multiple focus groups with people living with dementia in Northern Ireland were held to compare and contrast data between the groups. 20 people living with dementia participated in four focus group interviews. The researchers analysed the data using a thematic analysis.
What they found
1) Referring to the disabling aspects of dementia instead of the capabilities of someone living with dementia was a barrier to living well.
- Waiting to be re-tested for competence to drive after diagnosis
- Difficulty or anxiety about going shopping/banking/taking public. Small interventions such as a JAM card were noted as supportive in these activities.
2) Dementia should become more normalised “We don’t need a fool’s pardon”.
- Participants highlighted the benefit of better public understanding of dementia and the consideration of it as an illness like a heart condition or cancer.
- Local public health campaigns were seen as positive.
- Positive, informed media coverage, care to not encourage the stigma which surrounds dementia.
- Many were asked to give up work upon receiving a diagnosis. Support from employers and accommodation for the condition would have a very positive impact.
3) Dementia should not be viewed as a death sentence.
- Participants felt healthcare professionals needed to show more empathy and understanding and focus less on the symptoms and progressive incurable aspect of the condition.
- Family carers were seen as looking too far in to the future with a negative focus.
- Participants felt that there was a lot of life to live after a dementia diagnosis.
- Family members were identified as potential allies in the fight against stigma in the wider community.
What this means
Participants felt that society overlooks the life left to live by those diagnosed, despite efforts to improve public opinion. The focus group participants believed that better understanding of the condition in society, could enable people with a diagnosis to live a fuller, less restricted life.
Article Authors: Gary Mitchell, Victoria McTurk, Gillian Carter and Christine Brown-Wilson
Article reference: Mitchell.G, McTurk. V., Carter. G. & Brown-Wilson. C. (2020) Emphasise capability, not disability: exploring public perceptions, facilitators and barriers to living well with dementia in Northern Ireland, BMC Geriatrics, 20,(1).
Feb 2021: New Research Paper
Priorities for psychosocial supports and services among family carers of people with dementia in Ireland
Angela Miller from The ASI brings us a summary of a new research paper led by Áine Teahan.
Background
Dementia care relies heavily on family carers who often struggle with their own health and wellbeing. Aine Teahan from the National University of Galway and her colleagues wanted to identify personal and social challenges experienced by family carers of people with dementia and to find out what their needs are for a better support service from the government.
What the research team did:
A focus group was conducted in Kerry, Dublin and Galway, to find out the unique views and requirements of those living with and caring for people with dementia. They wanted to understand the personal and social needs of carers in families with dementia.
What they found:
The team examined individual and social supports and services. Interestingly, the top priorities were slightly different across the three areas.
Top Priorities for each area:
- Dublin: Long break respite
- Kerry: Day care
- Galway: Family carer support groups.
| The top rated personal supports needed across the groups included | The top rated social supports needed across the groups included: |
Other top priorities included were family carer education programmes, a budget for personal care and case management. |
Other top priorities included were dementia specific hospital departments, financial aid for legal services and fair deal legislation. |
What this means
It is clear that more Government investment is required in personal and social supports for carers, most urgently day care and non-means tested allowance. This would not only help to maintain family carers’ contributions to community-based care in dementia but would also facilitate social inclusion, social connectedness and economic sustainability.
Article Authors: Áine Teahan, Patricia Carney, Suzanne Cahill and Eamon O’Shea
Article Reference: Teahan Á, Carney P, Cahill S, O’Shea E. Establishing priorities for psychosocial supports and services among family carers of people with dementia in Ireland. Dementia. January 2021. doi:10.1177/1471301220984907

While ageing-in-place policies are gaining momentum in Ireland, actual investment in community-based care lags behind particularly in relation to family care. It is well-established that family carers experience deceased physical, mental and financial well-being while caring for a person with dementia. Increased investment in family carer supports is necessary to support the welfare rights of both family carers and of people with dementia, as well as create sustainable community-based care systems
Áine Teahan, Lead Author, National University of Ireland Galway
Kathleen Quinlan - Why I take part in research

“I’m Kathleen, I am 54 years young with two children and one grandchild. I was diagnosed with dementia in 2018.
I am passionate about research and I think it’s really important for people living with dementia to get involved in different projects.
Research into dementia is really important not only to find treatments, but also to improve our lives on a day to day basis.
When I take part in research I feel recognised as a person who is capable of doing things. I feel valued and that my self esteem is boosted. I enjoy talking about my feelings and experiences. I learn from research, it’s something to do, and I find it enjoyable too!
If you are thinking about taking part in research, have a go – I really recommend it!”
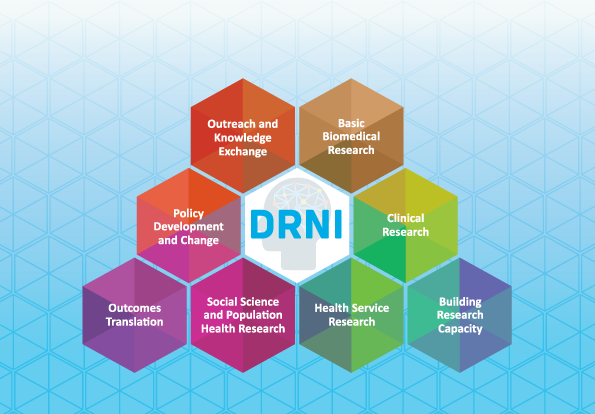
January 2021: Dementia Research Network Ireland: Prevention: Cure & Care for Dementia & Neurodegeneration
Dementia Research Network Ireland (DRNI) is a network of researchers, medical professionals, people living with dementia & Parkinson’s disease, and carers. There are over 100 members in the network, and all are involved in or have an interest in brain research. The network is funded by the Health Research Board.
Work by network members helps us to understand the causes of dementia, how to best care for people living with dementia and how to improve people’s quality of life. Network members come from disciplines such as social care, psychology and medicine. By working together in a collaborative way, this strengthens the research projects that are carried out.
DRNI members often conduct research which involves people living with dementia, carers and healthy members of the public. TeamUp For Dementia Research helps to match researchers with people interested in taking part in these research projects.
For more information about our research network:
Visit our Website: http://dementianetwork.ie/
Twitter: @drnire
Email: [email protected]
Phone: 086 145 1068
December 2020: FDA Reviewing New Alzheimer's Drug
What’s happening?
Biogen Inc. is an American multinational biotechnology company based in Cambridge, Massachusetts. On July 8th 2020, Biogen announced that it has submitted a Biologics License Application to the FDA (Food & Drug Administration) for aducanumab as a treatment for Alzheimer’s disease. The FDA has agreed to review the application under their priority review process and a decision is expected by June 2021.
Why does this matter?
It takes several years for drugs to get to this approval stage. If approved and effective, aducanumab could be the first treatment with the potential to meaningfully change the course of Alzheimer’s disease.
What is aducanumab?
Aducanumab is therapeutic antibody developed to clear amyloid plaques from the brain. Amyloid is a protein that builds up in the brains of people with Alzheimer’s Disease.
Clinical Trials Controversy
Biogen was testing aducanumab in Phase III clinical trials named EMERGE and ENGAGE. In these trials, Biogen was evaluating the impact of aducanumab on memory, thinking, and daily activities in people who had mild Alzheimer’s or Mild Cognitive Impairment (MCI). They were also testing the safety of the drug.
In May 2019, Biogen announced that it would stop these trials because they were not showing any sign of benefit to people with Alzheimer’s Disease. They did not see any significant safety concerns.
Five months later, Biogen took a u-turn. They reported that they some data in the EMERGE trial showed slower cognitive decline when participants took the highest dose across the whole treatment period. Biogen now believes aducanumab might slow the progression of Alzheimer’s Disease for some people.
Experts have warned that the interpretation of the data is tricky and we should be cautious. It’s clear that aducanumab can help remove amyloid from the brain but whether that slows cognitive decline is another question.
What is the FDA & CDER?
The mission of FDA’s Center for Drug Evaluation and Research (CDER) is to ensure that drugs marketed in this country are safe and effective. CDER does not test drugs, but it does conduct limited research in the areas of drug quality, safety, and effectiveness.
FDA approval of a drug means that data on the drug’s effects have been reviewed by CDER, and the drug is determined to provide benefits that outweigh its known and potential risks for the intended population.
What happens now?
The FDA is reviewing the application and a decision is expected by June 2021.
Often, there are issues that must be resolved before approval; the review team may request further data before they make a final decision.
If aducanumab receives FDA market approval it can then be prescribed in the USA. However, this can be significantly delayed depending on patents, manufacturing issues, the use of controlled substances in the drug etc. If aducanumab goes to market, there will be continuous follow up monitoring in a further clinical trial for safety reasons.
Biogen are also in talks with the relevant authorities in Europe and Japan about aducanumab.
